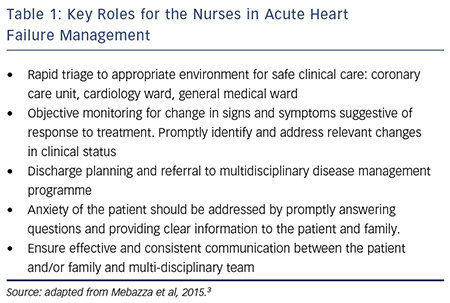
The specialised role of the heart failure nurse rose to prominence during the 1990s. Studies of heart failure disease management reported a reduction in the risk of hospital readmission in services with structured follow up that focused on the optimisation of therapy, out-patient follow up, education for self-care and the coordination of care.1 Nurses had already established their role in the long-term management of patients with chronic disease and quickly confirmed their role within heart failure disease management services. Such level of care became recognised in international guidelines and as a marker of a quality service.2 More recently there has been a developing interest in optimising patient outcome through a greater focus on the in-patient admission, faster diagnosis of acute or decompensated heart failure, in-patient management in an appropriate care environment and planned discharge which includes referral to a heart failure disease management programme. Recent recommendations for the early in-patient period acknowledge the clear roles for the nurse in the heart failure team and discussed in this article (Table 1).3
Immediate Assessment and Triage
From a patient perspective, the acute heart failure journey generally starts with increasing shortness of breath, sometimes accompanied by non-specific signs and symptoms of oedema, fatigue, loss of appetite and changes in weight. Patients seek professional help when their own self-care resources fail or through the encouragement of family or friends. For some, the onset of symptoms is rapid.4 Either way, patients generally have worsening shortness of breath when they present to a hospital emergency department. The UK National Heart Failure Audit provides a detailed picture of the patient admitted to hospital. It reports that almost 80 % of those admitted to hospital with acute or decompensated heart failure present with shortness of breath on at least moderate exercise during their first hospital admission: New York Heart Association (NYHA) III 44 %, NYHA IV 35 %.
At subsequent hospitalisations, the proportion of patients presenting with severe shortness of breath increases modestly: NYHA III 44 %, NYHA IV,40 %.5 On arrival in the emergency department, prompt recognition, management and transfer to an appropriate environment for care are necessary to alleviate both the physical and emotional symptoms of breathlessness and optimise outcome. Unlike the focus on triage of the patient presenting with acute-onset chest pain, emergency departments do not generally have an acute heart failure triage nurse. Therefore the initial patient triage is frequently undertaken by a nurse practitioner who elicits the patient history, assesses the severity of the clinical status and refers to the relevant team. In this way, such nurses play a key role within the multi-professional team by helping to distinguish the cause of breathlessness and initiating prompt symptom relieving therapy.
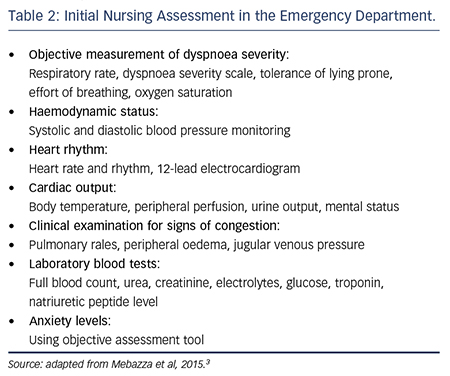
Key issues in the nurse’s initial clinical assessment of suspected acute heart failure are summarised in Table 2 and adapted from the most recent recommendations on management.3 Nurse practitioners generally have an ‘expanded’ skill set that enables them to also perform clinical examination to identify signs of congestion and refer for chest X-ray. Identifying clinical stability is an important first step in triage and enables the prompt transfer of the patient to the appropriate level of care for safe and effective therapy. This is largely influenced by the local organisation of services and skill sets of ward nurses. However, a patient at high risk of clinical deterioration or one requiring invasive cardiopulmonary support should ideally be transferred to the emergency resuscitation area, or an intensive or coronary care unit offering a lower patient-to-nurse ratio, closer patient monitoring and medical staff more available to support decision making.
Ongoing Monitoring and Management
The management of acute breathlessness or cardiopulmonary instability is generally carried out simultaneously with diagnosis. Once the diagnosis of acute heart failure is made, diuretics are administered to relieve dyspnoea. Ideally the dose should be the lowest needed to reduce fluid congestion and so balance the positive action with any potential negative effect on renal function. Close monitoring of renal function, fluid balance and urine output are therefore needed. There is often a tendency to assume urinary catheterisation for the close monitoring of urine output. However, urinary tract infection attributed to urinary catheterisation is the most frequent cause of hospitalacquired infection and in acute hospitals may account for as many as 20 % of all hospital-acquired infections. Risk increases the longer a catheter is in situ, with a daily risk estimated as between 3–7 %.6 This risk is likely to be increased further in the older adult with more health problems.
The consequences of such an infection are likely to vary, increasing the risk of a prolonged hospital stay and the development of in-hospital confusion, particularly in older adults. Alongside nursing actions to prevent infection, good practice also includes limiting the use of urinary catheters and, when they are necessary, removal as soon as possible. National and international guidelines suggest best practice in their use.7,8 In the context of acute heart failure this guidance can be interpreted to suggest urinary catheterisation should be restricted to those patients with cardiopulmonary instability and low cardiac output, when hourly urine output monitoring is needed.
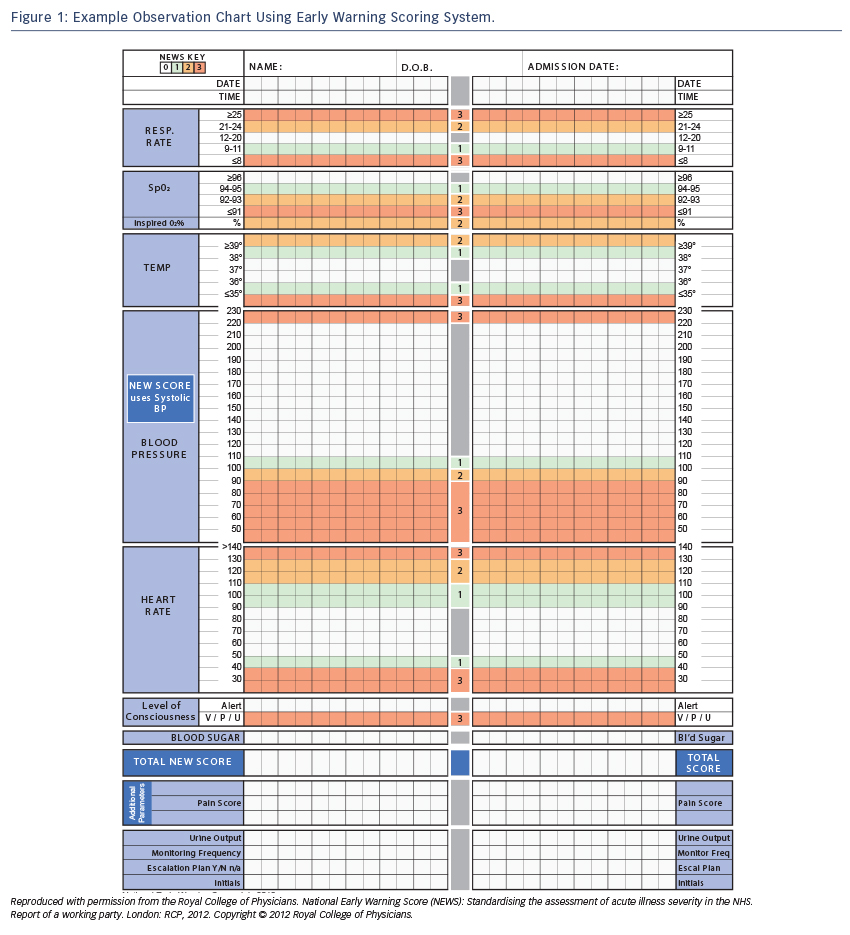
The ongoing monitoring of response to treatment and cardiopulmonary status also necessitates close monitoring of key haemodynamic parameters. In the immediate period of stabilisation, overly aggressive management with diuretics and vasodilators may lead to hypotension. Equally, patients may be undertreated or their underlying condition may deteriorate. Early warning scores allocate and weight points to vital signs outside pre-agreed ranges. These points are then summed to provide a single composite score. An increase in score will identify those patients who will benefit from escalation of monitoring or treatment. For example, they may benefit from an increased frequency of observationor ugent medical review. Escalation of treatment and alterations in management are then made in line with the ‘score’. To provide standardisation and limit misunderstanding the UK has adopted the National Early Warning Score (NEWS)9 (see Figure 1) for use in routine recording of clinical data, replacing traditional observation charts. Such tools have been reported to improve the ability of ward staff (both nursing and medical) to identify and respond to indicators of clinical change.10
Close monitoring requires a care environment where nurses have the time and expertise to identify and respond appropriately to changes in physiological data. The association between the competence of nurses and quality of care has long been recognised and more recently the association between nurse staffing, nurse expertise and patient outcome has been confirmed. A study of more than 400,000 patients in 300 acute hospitals in nine European countries reported an association between an increase in the number of nurses and the risk of death. An increase in a nurse’s workload by one patient increased the likelihood of a patient dying by 7 % (OR 1.068, 95 % CI [1.031–1.106]). Conversely, the risk of death was reduced where patients were cared for by academically prepared nurses; every 10 % increase in the number of bachelor-degree nurses on the ward decreased the likelihood of death by 7 % (OR 0.929, 95% CI [0.886–0.973]).11 The authors concluded that patients in hospitals in which 60 % of nurses held bachelor degrees and in which the nurse-to-patient ratio was 1:6 would have an almost 30 % reduced risk of death than patients in hospitals in which only 30 % of nurses had bachelor degrees and each cared for eight patients.11
Within the context of heart failure the UK National Heart Failure audit revealed that in-hospital mortality is lower when patient care is managed in specialist cardiology wards rather than general medical wards (7.8 % versus 13.2 %).5 Taken together these papers suggest that outcome is improved when in-patient care is provided by a specialised team and by ward nurses familiar with the management of heart failure. Countries will need to decide locally how to interpret and implement these findings but they point to an association between the quality of nursing care and patient outcome.
It is not always possible for every patient to receive in-patient care on a specialist cardiology ward and some will be best cared for on general medical or care-of-the-elderly wards where nursing staff have specific expertise in managing the care needs of the frail, older adult. The heart failure management of the older adult is complicated by concomitant comorbid conditions, altered pharmacokinetics, frailty and cognitive impairment. Consequently their hospital length of stay is likely to be longer and also influenced by the availability of post-discharge social support. The UK National Audit data reports an increased length of stay (LOS) in heart failure patients not cared for on cardiology wards and this relates to the majority of those patients aged above 74 years (mean LOS 12.7 days (cardiology ward) versus 13.1 days (general medical) and 14.7 days (other ward areas)).5
The in-patient hospital stay allows review of all medication, as well as combinations that may increase the risk of side effects. The in-patient admission also provides time for the safe introduction of new heart failure medication and this is likely to be slower in the older patient. When accompanied by close monitoring of physiological variables and assessment of the patient’s ability to manage potential effects, such as lower systolic blood pressure or increased diuresis, the in-patient stay can increase the safe prescription of medication, as well as positively influence patient compliance. For example, nurses can remind patients to stand up slowly to reduce their risk of dizziness and falls, teach them to modify the timing of diuretics to enable activities outside the home and facilitate the supply of continence aids when necessary. Where in-patient care is not provided on a cardiology ward this can be facilitated by regular outreach by the heart failure team and the heart failure specialist nurse has a central role in this, providing advice, education and liaison between the health-care teams directly involved in providing care and the heart failure specialist team.
Regardless of the place care is delivered, ideally patients with heart failure should be identified and followed up during their hospital stay by a specialist heart failure team. Using medical admission records the heart failure specialist nurse can identify patients with suspected heart failure, act as a point of contact for advice and ensure appropriate discharge planning and follow up. Once stabilised patients should be started or restarted on evidence medicines. Various models for such outreach exist but the exact model will depend on the local organisation of care.12
Discharge Planning
In-patient management extends beyond haemodynamic monitoring and initiation of medication to planning for discharge and the smooth transition to a community heart failure disease management programme. It is now well recognised that patients are at high risk of hospital re-admission during the first few months following discharge. This has led to recommendations for follow up early in the postdischarge period and ideally within the first one to two weeks.3 Disease management programmes are now established in many European countries. A recent survey of countries of the ESC reported that heart failure clinics are present in 75 % of those countries that completed the survey and that a heart failure nurse specialist was employed in the majority of those clinics.13
Discharge planning commences once the patient is stabilised and discussions include the heart failure specialist team, the patient and, where necessary, the patient’s family. Preparing for discharge requires assessment of social environment into which the patient will be discharged as well as their capacity to self-care. Patients admitted to hospital with heart failure are frequently elderly with multiple comorbidities. They have reduced physiological reserve to adapt to change and stress and may require a period of rehabilitation and supportive community resources in the initial post-discharge phase. In such situations the heart failure nurse co-ordinates discussions to develop a collaborative discharge plan. In a quasi-experimental study in Sweden of 248 elderly patients hospitalised with heart failure Ulin and colleagues report an earlier hospital discharge in patients whose discharge plan was a collaborative process between the heart failure team and social/community team. They report a mean of 6.7 in-hospital bed days compared with 9.2 days in patients who did not receive a co-ordinated discharge plan.14 Such an approach may have particular advantage when hospital discharge is delayed due to social circumstances.
Regardless of age, discharge from hospital is frequently cited as a period of high anxiety for both patients and their families. A coordinated care plan that estimates time to euvolamia and commencement of heart failure medication can be communicated and discussed at an early stage and so help prepare both the patient and their family for discharge.
Patient Education
The in-hospital period is also an ideal time to provide education about heart failure, its monitoring and management. It is possible that some hospital admissions are preventable if worsening heart failure is recognised early; some patients and family wish to be involved in self-care e.g. by monitoring their condition, recognising significant change and taking appropriate action. They should be introduced to these concepts during the in-patient stay. There is often a mismatch between a patent’s understanding of their heart failure management and the information provided by the health professional. For example, the Euroheart failure survey reported that patients recalled only 46 % of the self-care advice given15 whilst Ekman and colleagues, in a substudy of the COMET study, reported that adherence to medication was associated with patient beliefs about their medication.16
Results such as these point to the complexity of providing the patient with education for self-care and are recognised in the current focus on individualising patient education. A patient’s capacity to learn and retain new information may be reduced whilst hospitalised, in part due to higher levels of anxiety and cognitive dysfunction. It is therefore good practice to use the hospital admission to provide the patient with verbal information that is supported by written material. Some nurses use the ‘teach-back technique’ whereby they ask the patient to repeat, using their own words, the information they have given them.17 This enables the patient to confirm their understanding and the nurse to rephrase any information that is misunderstood. Such a technique involves the nurse and patient in the repetition of information and increases the time the nurse spends with the patient discussing heart failure and its management. It is possible that this increased time spent in patient education provides benefit in terms of knowledge retention and may be particularly valuable when interacting with the person with low educational or health literacy. Both the education provided and the patient’s understanding should be communicated to the heart failure disease management team and should form a basis for ongoing education and support.
End-of-life Care
Mortality is high in patents discharged from hospital following an acute heart failure admission. Despite advances in care about 14 % of patients still die within six months of hospital discharge.18 Various factors are likely to increase this risk such as age, frailty, number of hospital admissions in the preceding 12 months and presence of cachexia.2 The hospital admission provides time to identify patients with a worse prognosis and introduce palliative and supportive measures. Such care actions include providing pain relief, discussions around future care planning and preferred place of death. There is a growing recognition of the need for such discussions and hospitals increasingly provide a palliative care service jointly between the heart failure and palliative care nurse. Where such services exist studies report a reduction in symptom burden and depression and improvements in quality of life.19 Such services also report an increase in advance care planning.20 This may help address the currently reported mismatch between patients’ preferred and actual place of death.
Conclusion
Patients with acute heart failure benefit from early diagnosis, close monitoring and management provided by skilled heart failure teams that include a heart failure nurse specialist and by cardiology ward nurses with sufficient education to support safe practice. As part of the team, the heart failure nurse specialist is well placed to also provide an outreach service to patients throughout the acute heart failure pathway and this requires close collaboration with nurses in non-cardiology specialist areas such as the emergency department and general medical/care-of-the-elderly wards. In contrast to the evidence base to support the heart failure nurse in long-term disease management, the nurse’s role in the acute heart failure pathway is less clearly defined. We now need to turn our attention to this in-patient period and strengthen the evidence that supports the role, number and skill set required of nurses to underpin effective heart failure treatment throughout the entire patient journey.